The Better Health, Better Living project, one of the regional winners in the HMI Leaders Award, is the implementation of the Chronic Disease Self Management Programme (CDSMP) at Beaumont Hospital, Dublin, in co-operation with multiple patient organisations and HSE stakeholders, writes Ms. Marese Heffernan, Co-ordinator of the project.

The project run by Dr. Jennifer Wilson O’Raghallaigh and Ms. Mary Forry and developed by Stanford University, is a psycho-educational mixed conditions workshop delivered weekly for 2.5 hours over six weeks.
Chronic disease takes an enormous toll on people’s lives. It causes pain, disability, decreased physical activity, and poor emotional health, which can seriously compromise the quality of daily life.
Eighty to ninety percent of all care for people with chronic conditions is undertaken by people themselves and their families (Health Service Executive, 2008). By effectively promoting the self management of our patients in addition to the care they receive from our direct services, we were trying to achieve an improvement in their health, activity levels, quality of life and mood that is cost effective, sustainable, and applicable to patients across the hospital setting. We also sought to develop and support a programme that could be used in hospital or community settings to strengthen our links with community and patient organisations, and to support our colleagues in primary care.
To date over 100 patients have been through this programme and learned valuable skills and techniques to assist them in becoming better self-managers of their illness.
Throughout the programme participants learn techniques to deal with problems such as frustration, fatigue, pain and isolation,exercise methods, communicating effectively, nutrition, relaxation, appropriate use of medication and decision making in medical care. Such techniques are learned through setting weekly action plans (weekly goals), group discussions, manualised educational ‘lecturettes’, and leader modelling.
Importantly, sessions are delivered by two leaders, one of whom must be a patient volunteer with a chronic illness who has undergone certified leader training over four full days. The second leader may be either a health-care professional trained in the same way, or another trained patient volunteer. The fact that this is a peer led programme significantly enhances its transferability as any community with an active volunteer network can successfully deliver this programme.
Stanford University designed this programme so that it could be delivered in community settings. Minimal materials are required i.e. chart paper, markers, group space. Thus, once trained leaders are available, the programme can successfully be delivered in community settings. Members of our MDT, Dr. Jennifer Wilson O’Raghallaigh and Ms .Mary Forry, as well as two patient volunteers have been successful in achieving master trainer certification from Stanford University allowing this project to continually train new CDSMP leaders, strengthening the programme’s sustainability. Over 50 volunteer leaders, a mixed group of both patient leaders and healthcare professionals from various organisations have successfully completed training to lead the CDSMP.
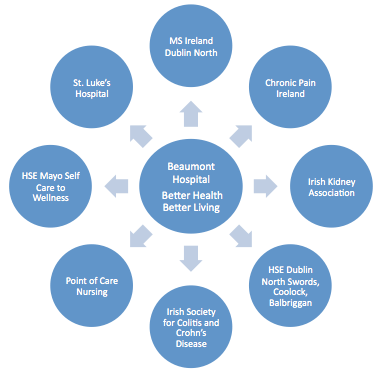
The MDT is keenly aware that delivering this programme in a community setting would decrease the demand on hospital resources. Accordingly the project has been actively establishing links with community partners in the Dublin area and on a wider national basis with the aim of developing a system of delivering regular programmes in communities across the country. Fortunately the project has been very successful in establishing such valuable links with patient organizations, e.g. Irish Society of Colitis and Crohn’s Disease, Chronic Pain Ireland, St. Luke’s Oncology Service and MS Ireland. Below is a visual representation of the links established between Beaumont Hospital’s Better Health Better Living and various patient and community organisations, again demonstrating the sustainability of the programme beyond hospital settings.
To date over 100 patients have been through this programme and learned valuable skills and techniques to assist them in becoming better self-managers of their illness. Most importantly there have been significant improvements in patient outcomes. Regarding quantitative outcomes, results from a preliminary pilot study conducted by members of the MDT showed significant improvements in participants’ health related quality of life, as well as reductions in anxiety and depression, with gains maintained at 3 month follow up. These findings are in line with international research findings on the CDSMP.
In terms of qualitative outcomes this project has received overwhelmingly positive feedback from participants who describe an overall improvement in their experience of managing their health condition. Participants consistently report feelings of empowerment and improved self-confidence, e.g.
“I learned to set achievable targets or goals for the week ahead…. Once you have reached your target there is a great sense of accomplishment and pride.”
Another common theme reported by participants was the welcomed social support provided by other participants who have experienced similar difficulties, e.g.
“It was a relief telling things about myself to people who have gone through similar and are able to understand these things the way most people don’t”
By continuing to evaluate these benefits and through the regular recruitment and training of new volunteer leaders, as well as the active engagement of local community resources and development of a strong organisational network, we hope to ensure that patients with chronic conditions have maintained access to an evidence-based, peer-led self-management intervention.

