Mary Hickey explains how “lean” helped to improve the flow in the Trauma Orthopaedics OPD Department, in the Adelaide & Meath incorporating the National Children’s Hospital in Tallaght.
This lean project was instigated in order to manage patient waiting times and “level the load” in the Trauma Orthopaedic Out Patients department. One of the main reasons to undertake this project was the clinic staff view that it could take patients anything from 45 minutes to three and half hours to complete their episode of care in this clinic which has a complex case – mix. We decided to undertake a Kaizen event to address this issue.

Kaizen is the Japanese name for continuous improvement. A Kaizen event or “rapid improvement” event is a core element of the lean approach. A cross functional team is formed specifically for the event. There are three phases to conducting a Kaizen event:
- Stage 1. Planning event – 2 to 4 weeks
- Stage 2. A workshop – 3 to 5 days
- Stage 3. Follow up Phase – Report Outs at 30/60/90 days
In order to manage this specific Kaizen, a representative group of clinic staff which included medical, nursing, allied health, radiography and clerical staff were invited to participate in the event. Facilitation was provided by a lean expert. A project sponsor (the orthopaedic clinical lead) was agreed and support was sought and received from the CEO and Director of Nursing.
Patient feedback was very positive with 88 per cent rating the service as “good” or “very good”
The team mapped the “current state” process and then proceeded to discuss what the “future state” should look like and how to achieve this new reality. A change to the clinic time slots was agreed – 30 minute intervals with a specified number of new and return patients. The clinic was also capped at 80 patients. Complex patients requiring additional time were identified by attaching a coloured dot to their medical chart. Ward and clerical staff were informed of the changes in appointment booking practices.
Implementation
A tracking sheet was created and clipped to the outside of the chart. This signalled the patients’ journey through the clinic and the duration of each interaction. Changes were made to the design of the nurses’ station and a magnet board was introduced to manage the clinic flow. Patients were given a number when they registered at the clinic and this number equated to a number on a magnet which was moved on the magnet board once the patient handed in their chart at the nurses’ station.
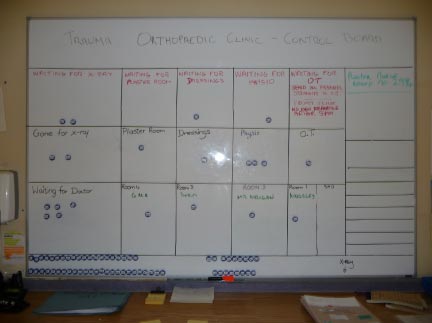
The team developed a procedure for the management of the board. The nursing staff moved the magnet as the patient moved through the clinic. Staff were also able to see if there was any congestion in the process and manage accordingly. Importantly, it also acted as a communication tool for patients as they could see at a glance where they were in the process and the number ahead of them.
Patient feedback was very positive, with 88 per cent rating the service as “good” or “very good”. They felt that the system was transparent and that they were seen in an orderly fashion with no one jumping the queue.
Other issues identified during the mapping process were the delays in radiology and the plaster room. It was agreed that two radiographers and two plaster nurses would be assigned for the duration of the clinic. Improved documentation of the patients’ treatment plan in their chart eliminated the need for separate referrals to physiotherapy, occupational therapy and the plaster room.
Visual displays were developed, including reminders for patients to arrive on time for follow up appointments, to reschedule appointment if unable to attend and to arrange a follow up appointment before leaving clinic as per their treatment plan. A patient information leaflet was devised and given to patients in the Emergency Department when they received their initial referral.
Conclusions
A patient’s experience may be a simple pathway involving two disciplines or a complex pathway requiring interventions by up to six different disciplines. Patients on these various pathways were distributed throughout the clinic in order to level the load. This, in addition to the improvements outlined above, resulted in a significant reduction in the average wait and the range of wait times across the clinic.

